What is Eczema?
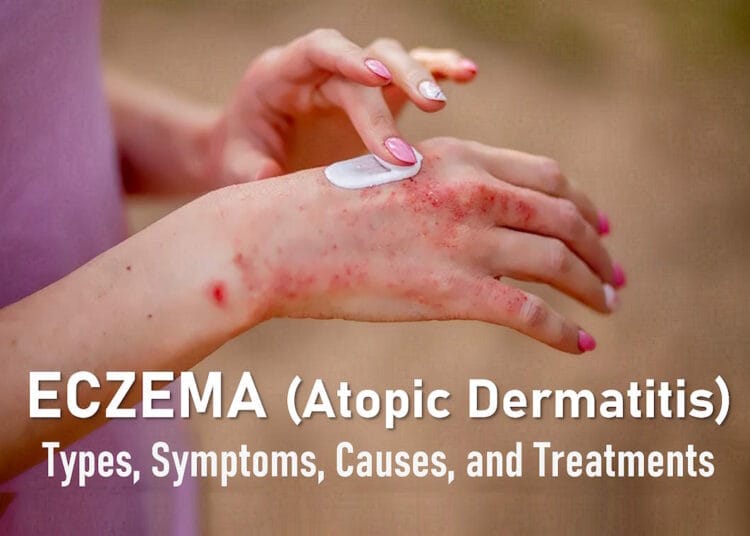
Eczema refers to a group of inflammatory skin conditions characterized by itching, dry skin, rashes, scaly patches, blisters, and skin infections. There are seven distinct types of eczema: atopic dermatitis, contact dermatitis, dyshidrotic eczema, nummular eczema, seborrheic dermatitis, and stasis dermatitis. On lighter skin, eczema may appear red and inflamed, while on darker skin tones, it can present as brown, purple, gray, or ashen. The hallmark symptom of eczema is persistent itching.
Over 31 million Americans live with some form of eczema. It can develop during childhood, adolescence, or adulthood and vary in severity. In newborns, eczema may emerge within the first few weeks or months of life, often presenting as dry, itchy patches that can become infected due to excessive scratching. Adults commonly experience eczema in their 20s or later in life, particularly after age 50.
Eczema flare-ups, periods of intensified symptoms such as itching and redness, are common. Many individuals use moisturizers, antihistamines, topical steroid creams, and corticosteroids as part of their eczema treatment. Severe eczema flare-ups can persist for weeks, causing complications such as skin infections or an increased risk of conditions like asthma and food allergies, often referred to as the “Atopic March.”
Getting an accurate diagnosis is essential, as eczema can sometimes be mistaken for other skin conditions, like psoriasis. Consulting a dermatologist or healthcare provider ensures proper treatment and helps manage symptoms effectively.
What is Atopic Dermatitis?
Atopic dermatitis, often called “atopic eczema,” is the most common form of eczema. It occurs due to an overactive immune system that weakens the skin’s protective barrier, leading to dryness and itching. Eczema is not contagious—you cannot catch it from someone else. Although the exact cause is unknown, experts believe eczema results from a combination of genetic and environmental factors.
Many individuals with atopic dermatitis also experience hay fever, allergic asthma, or food allergies. Consistent skin care is vital in preventing flare-ups and managing symptoms effectively.
What Causes Eczema?
There isn’t a single cause of eczema. Instead, the condition is linked to various factors, including genetics, environmental triggers, and immune system responses. Each of the seven eczema types may have unique causes, but some common contributors include:
Overactive Immune System
Atopic dermatitis occurs when an overactive immune system responds to irritants by triggering inflammation. This leads to dryness, itching, and redness on the skin. Symptoms can appear on any part of the body, especially in areas where skin creases, such as behind the knees, elbows, and lower legs.
Genetics
Genetics also play a role in eczema development. For instance, a deficiency in filaggrin—a protein that helps the skin retain moisture—can lead to dryness and irritation. If you have a family history of eczema, your risk of developing the condition is higher.
Environmental Triggers
Exposure to certain environmental factors can provoke eczema flare-ups. Common triggers include:
- Dry air or extreme temperatures
- Harsh soaps, shampoos, and bubble baths
- Laundry detergents and fabric softeners containing chemicals
- Irritating fabrics like wool or polyester
- Surface cleaners and disinfectants
- Juices from fruits, vegetables, or meats
- Fragrances in candles and personal care products
- Metals like nickel in jewelry or utensils
- Formaldehyde in household disinfectants and adhesives
- Isothiazolinone, found in some baby wipes and skincare items
- Thickening agents like cocamidopropyl betaine in shampoos
- Dyes such as paraphenylene-diamine in temporary tattoos
- Dust mites and unclean environments
Stress
Emotional stress can also exacerbate eczema symptoms, though the exact mechanism remains unclear. Some individuals experience heightened flare-ups during stressful periods, while others become stressed due to the discomfort of their eczema, creating a cycle of worsening symptoms.
Is Eczema Contagious?
Eczema is not contagious—you cannot catch it or pass it on to someone else. While the exact cause of eczema remains unclear, researchers have determined that it develops due to a combination of genetic predisposition and environmental triggers.
What Are the Symptoms of Eczema?
One of the key things to understand about eczema is that its symptoms vary from person to person. Your skin’s response and the specific areas affected may differ from someone else’s experience, even within the same household. Additionally, different types of eczema may appear on distinct parts of the body at various times.
Itchy skin, scientifically termed “pruritus,” is a hallmark symptom of eczema. The intensity of the itch can range from mild to severe. In some cases, the itching becomes so intense that scratching leads to broken skin and bleeding, which is referred to as the “itch-scratch cycle.”
Common symptoms of eczema include:
- Itching
- Dry, sensitive skin
- Inflamed or discolored skin
- Rough, leathery, or scaly patches
- Oozing or crusting
- Swelling
You may experience all or only a few of these symptoms. Eczema can present differently based on skin tone, appearing red and inflamed on lighter skin and as ashen, gray, brown, or purple on darker skin tones. Severe eczema symptoms, such as those reported by many Black Americans, can lead to significant discomfort. Consulting a dermatologist is the best way to confirm if you have eczema and to develop an effective management plan.
Eczema is sometimes mistaken for other skin conditions like psoriasis, though they are distinct disorders. People with eczema often report additional allergic conditions, such as hay fever, asthma, and food allergies.
How Many Types of Eczema Are There?
There are seven main types of eczema, each with unique characteristics. Symptoms, causes, and treatments often overlap, making it challenging to differentiate between types. Below is an overview of the most common forms of eczema:
1. Atopic Dermatitis
The most prevalent type of eczema, atopic dermatitis, affects over 9.6 million children and 16.5 million adults in the United States. Intense itching is its primary symptom, which can disrupt sleep and lead to other complications such as painful rashes and weakened skin barriers. This type of eczema can appear anywhere on the body and may result in oozing rashes.
2. Contact Dermatitis
Contact dermatitis occurs when the skin becomes inflamed or irritated after exposure to specific substances. While it shares common eczema symptoms, the defining feature is its reaction to environmental triggers, such as chemicals or allergens.
3. Dyshidrotic Eczema
Dyshidrotic eczema is characterized by small, itchy blisters on the hands, feet, and edges of the fingers and toes. Often referred to as “hand eczema” or “foot eczema,” this type’s exact cause is unknown, but it tends to affect men more frequently than women.
4. Neurodermatitis
Neurodermatitis causes intense itching, often resulting in thickened, scaly skin due to excessive scratching. Discolored patches are common and can appear on the feet, ankles, hands, wrists, elbows, shoulders, neck, and scalp.
5. Nummular Eczema
Nummular eczema, also known as discoid eczema or nummular dermatitis, presents as circular, coin-shaped patches of irritated skin. These patches may ooze or feel extremely dry and sensitive.
6. Seborrheic Dermatitis
Seborrheic dermatitis primarily affects the scalp, causing persistent itching and rashes. It can sometimes extend to other oily areas of the body, such as the face. Specialized shampoos are often recommended as a treatment option for managing this condition.
7. Stasis Dermatitis
Stasis dermatitis, also called gravitational dermatitis or venous stasis dermatitis, occurs when poor circulation in the legs leads to skin irritation. Symptoms are typically limited to the legs and include itchy, discolored, and dry skin. On darker skin tones, affected areas may appear brown, purple, gray, or ashen, while on lighter skin, redness is more common.
Atopic Eczema Treatment
Treating atopic eczema typically involves three main approaches:
- Avoiding skin irritants and other triggers whenever possible.
- Using moisturizers (emollients) daily to help prevent inflammation.
- Applying topical steroid creams or ointments to reduce inflammation during flare-ups.
Avoid Triggers and Irritants
Flare-ups may occur unpredictably, but certain triggers can worsen eczema. To minimize flare-ups:
- Avoid soaps and bubble baths that dry out the skin. Use soap substitutes and bath/shower moisturizers instead.
- Be cautious with biological washing powders and fabric conditioners as they may irritate the skin.
- Keep nails short and discourage scratching. For infants, use anti-scratch mittens.
- Opt for cotton or smooth fabrics next to the skin rather than wool or other irritating materials.
- Avoid extreme temperatures, as they can aggravate eczema symptoms.
- Rinse clothes thoroughly after washing to remove detergent residues.
Avoid Food Allergies
Approximately half of children with atopic eczema have a food allergy that exacerbates their symptoms. Common allergens include cow’s milk, eggs, soy, wheat, fish, and nuts. If a food allergy is suspected:
- Consult a doctor for guidance.
- Maintain a food and symptom diary for 4–6 weeks to identify potential triggers.
- Have food allergies confirmed by a specialist before eliminating any foods.
Dietary modifications may be recommended for severe eczema that is unresponsive to other treatments.
Use Moisturizers (Emollients)
Emollients are essential for managing eczema. These products moisturize the skin, prevent dryness, and reduce itchiness and flare-ups. Examples include lotions, creams, ointments, and bath/shower additives.
Important Safety Note: Some emollients contain paraffin or other oils, which are flammable. Oils from emollients can accumulate on clothing and bedding, creating a fire risk. Avoid exposure to naked flames, including cigarettes, and do not smoke in bed.
General Tips for Using Emollients:
- Thicker, greasier ointments are more effective and longer-lasting than lighter creams but can be messier to apply.
- Apply emollients liberally to all areas of the skin. They are safe to use as often as needed and are not absorbed into the bloodstream.
- Apply in the direction of hair growth to avoid blocking hair follicles.
- Use emollients daily, even when the skin appears healthy, to prevent flare-ups.
- Consider bath additives or shower gels as a supplementary measure for extensive dryness. However, these should not replace creams, ointments, or lotions applied directly to the skin.
- Pump dispensers are preferable to pots, as they reduce the risk of contamination. If using a pot, always use a clean spoon or spatula to remove the product.
Sample Routine for Moderate Eczema:
- Add an emollient oil to your bath water or use it in the shower for a base layer of moisture.
- Use a thick emollient ointment as a soap substitute and apply it to especially dry areas.
- After bathing or showering, pat the skin dry with a towel and apply an emollient cream or ointment to any remaining dry areas.
- Reapply emollients throughout the day as needed.
- Consider using dry dressings to keep emollients in place and prevent scratching (do not use if there is a skin infection).
- Apply a thick emollient ointment before bedtime.
Steroid Creams and Ointments (Topical Steroids)
Topical steroids are effective in reducing skin inflammation and are categorized into four potency levels: mild, moderately potent, potent, and very potent. The choice of steroid depends on the severity and location of the eczema.
Types and Uses
- Hydrocortisone cream 1%: A commonly used mild topical steroid.
- Creams: Best for moist or weeping areas.
- Ointments: Ideal for dry or thickened skin.
- Lotions: Useful for hairy areas like the scalp.
Typically, a course of topical steroids is used during flare-ups and continued until symptoms completely resolve. Most flare-ups clear within 7–14 days, though some cases may require longer treatment. The frequency and duration of use vary by individual.
General Guidelines
- Start with the lowest potency steroid that effectively clears the flare-up.
- If no improvement occurs after 3–7 days, a stronger steroid may be prescribed.
- In severe cases, a potent steroid may be recommended from the outset.
- Use different potencies for different areas, e.g., mild steroids for the face and stronger steroids for thicker skin on arms or legs.
High-Strength Steroids and Short Burst Therapy
For adults, a short three-day course of a potent steroid may be an alternative for treating mild-to-moderate flare-ups. This method can be quicker and more convenient while remaining safe for short durations.
Side Effects of Topical Steroids
Short courses (less than four weeks) are generally safe. However, prolonged or frequent use of potent steroids can lead to side effects:
- Skin thinning: Often associated with strong steroids under airtight dressings. Reversible if steroids are discontinued.
- Permanent changes: Stretch marks, bruising, discoloration, or spidery blood vessels with long-term use.
- Worsened skin conditions: Acne, rosacea, or perioral dermatitis.
- Systemic absorption: Rarely, strong steroids can enter the bloodstream, potentially affecting growth in young children requiring frequent treatments.
Recently, there has been growing awareness of topical steroid withdrawal (TSW), though it remains poorly understood and rare. TSW symptoms may include red, painful, peeling skin after discontinuing long-term use of potent steroids, particularly on delicate areas like the face. To minimize risk:
- Avoid prolonged, uninterrupted use of potent steroids.
- Use lower-strength steroids for sensitive areas.
Short-Duration Treatment to Prevent Flare-Ups (Weekend Therapy)
For individuals with frequent flare-ups, applying steroids to typical flare-up sites for two days per week (weekend therapy) may help prevent recurrences. This strategy often reduces overall steroid use over time. Discuss this option with your doctor.
Using Moisturisers and Topical Steroids Together
Most individuals with eczema are prescribed both emollients (for daily use) and topical steroids (for flare-ups). Proper application is crucial for effectiveness:
- Apply the emollient first and wait 10–15 minutes for it to be absorbed.
- The skin should feel moist or slightly tacky, not slippery, before applying the topical steroid.
Infected Eczema Patches
Eczema patches can become infected during flare-ups. Signs of infection include:
- Weeping blisters
- Infected skin lumps (pustules)
- Crusts
- Failure to respond to normal treatment
- Rapidly worsening eczema
If the infection becomes severe, symptoms may include fever and feeling generally unwell. In these cases, a course of oral antibiotics is typically prescribed alongside the usual eczema treatments.
Updated NICE Guidelines (2021)
The UK’s National Institute for Health and Clinical Excellence (NICE) offers the following guidance:
- Weeping blisters and crusted eczema do not always indicate infection.
- Antibiotics often do not significantly improve eczema outcomes, as most cases improve without them.
- Repeated antibiotic use increases the risk of antibiotic-resistant bacteria.
- Antibiotics are generally recommended only if the individual is unwell or feverish.
For infected eczema in otherwise healthy individuals, usual eczema treatments are typically sufficient. Doctors may recommend antibiotics in certain cases, such as for individuals at high risk of complications.
Skin swabs are generally not useful during eczema flares, as they cannot reliably distinguish between bacteria causing infection and normal skin bacteria. However, if eczema is infected by the herpes simplex virus, antiviral medication is necessary.
Post-Infection Care
- Dispose of all creams, ointments, and lotions used during the infection and replace them with new supplies to avoid contamination.
- If infections recur frequently, a topical antiseptic (e.g., chlorhexidine) may be advised to minimize bacteria on the skin, in addition to regular treatments.
What If the Eczema Treatment Doesn’t Work?
If a flare-up worsens or does not improve despite using emollients and topical steroids, consult your doctor. They may consider:
- Increasing the strength of the topical steroid
- Ensuring emollients are being applied often enough to maintain skin moisture
- Prescribing antibiotics if infection is suspected
- Checking for potential allergies to ingredients in creams, such as preservatives
Persistent or severe cases may require referral to a skin specialist for further evaluation and advanced treatment options.
Other Treatments for Atopic Eczema
Tacrolimus Ointment and Pimecrolimus Cream
These topical immunomodulators suppress specific cells involved in inflammation. Unlike steroids, they effectively reduce eczema-related skin inflammation and are licensed for individuals aged 2 years and older whose eczema is not well-controlled by standard treatments. Note: they should not be applied to infected skin.
Steroid Tablets
Short courses of steroid tablets may be prescribed for severe eczema cases that do not respond well to topical treatments.
Eczema Soaks
Eczema with weepy blisters may benefit from specialized soaks designed to dry the affected areas.
Hospital Treatments
Severe eczema cases might require hospital care, which could include treatments such as:
- Wet wraps
- Tar and/or steroid occlusion bandages
- Light therapy
- Immunosuppressive or immune-modifying medication
Tar Shampoos
These shampoos can help remove scaling from the scalp caused by eczema.
Antihistamine Tablets
Although not highly effective at reducing itch, certain antihistamines can cause drowsiness, making them useful for helping children with eczema sleep better at night.
Dilute Bleach Baths
Under medical supervision, diluted bleach baths can help clear bacteria from the skin and may be beneficial for children with chronic, hard-to-manage eczema. However, this treatment should only be done under the guidance of a healthcare professional, as improper dilution can cause serious harm.
Alternative Remedies
Some individuals try alternative remedies such as herbal medicines. However, caution is advised since some products may contain steroids or harmful substances, particularly if the labels are not clear or in a language you do not understand. Certain Chinese remedies, for example, have been associated with liver damage.
Preventing Atopic Eczema in Newborns
Breastfeeding a newborn for three months or longer may help prevent eczema in babies with a family history of allergies, such as hay fever or asthma. However, there is no evidence to suggest that mothers need to avoid specific foods during pregnancy or breastfeeding to reduce the risk of eczema.
Complications of Atopic Eczema
Atopic eczema can lead to various complications, including:
- Infected Eczema: As discussed earlier, infections can complicate eczema flare-ups.
- Mental Health Difficulties: The distress caused by eczema can affect daily life, self-confidence, and mental health, potentially leading to depression. Children may miss school or face bullying due to visible eczema symptoms.
- Sleep Problems: Itchy skin often disrupts sleep for both children and adults.
- Allergies: Individuals with eczema are more prone to hay fever, asthma, and food allergies. In infants, eczema may increase the likelihood of food allergies due to the immune system recognizing allergens that penetrate through compromised skin barriers.
- Changes in Skin Color: After healing, affected skin may appear lighter (post-inflammatory hypopigmentation) or darker (post-inflammatory hyperpigmentation) than surrounding areas. This is more common in people with darker skin tones and may take months to resolve.
Frequently Asked Questions (FAQs)
What is the best treatment for eczema?
The best treatment for eczema typically includes moisturizing the skin, using topical corticosteroids, and avoiding triggers that can cause flare-ups. In some cases, doctors may recommend topical immunomodulators or other medications. For severe eczema, systemic treatments such as oral steroids or biologics may be necessary.
What is the best eczema cream?
The best eczema cream depends on the severity and location of the eczema. Commonly recommended creams for eczema include corticosteroid-based treatments like hydrocortisone cream, as well as emollients or non-steroidal options such as tacrolimus or pimecrolimus. It’s essential to consult a healthcare provider to determine the right cream for your needs.
Can eczema appear on the face?
Yes, eczema can affect the face, particularly around the eyes, cheeks, and forehead. Facial eczema often results in redness, dry patches, and irritation. Mild topical steroids or emollient creams may be used to treat eczema on the face, but it’s important to avoid using strong steroids near the eyes.
How can I treat baby eczema?
Baby eczema is common and often appears as dry, itchy patches on the skin, typically on the face, elbows, or knees. To treat baby eczema, apply a gentle moisturizer frequently, use mild, fragrance-free soaps, and avoid triggers such as wool fabrics. If eczema persists or worsens, a pediatrician may recommend topical steroids or other treatments.
What is the difference between psoriasis and eczema?
Psoriasis and eczema are both skin conditions that cause redness and inflammation, but they have distinct characteristics. Psoriasis often results in thick, silvery scales, while eczema is more likely to cause dry, itchy, inflamed patches of skin. Psoriasis is primarily a condition of the immune system, while eczema is often triggered by environmental factors and allergens.
How do I treat scalp eczema?
Scalp eczema causes dryness, flaking, and itching on the scalp. Treatment usually involves using specialized shampoos containing ingredients like corticosteroids, coal tar, or ketoconazole. Gentle hair care practices, including using mild, fragrance-free products, can also help manage scalp eczema.
What is weeping eczema?
Weeping eczema occurs when the skin becomes so inflamed that it oozes fluid or pus. This can happen in more severe cases of eczema and may increase the risk of infection. Treatment involves using ointments to reduce inflammation and prevent further irritation, along with proper skin care to keep the area clean.
Can eczema affect the lips?
Yes, eczema can appear on the lips, causing dry, cracked, and inflamed skin. Lip eczema is commonly caused by irritants such as lip balms or flavored lip products. Treatment typically includes using gentle, hydrating lip balms and avoiding harsh ingredients that may trigger flare-ups.
How do I treat ear eczema?
Eczema can affect the ears, causing dry, itchy skin inside and around the ears. Topical corticosteroids and emollients are often used to treat ear eczema. It’s important to avoid inserting anything into the ear canal and to follow a proper skincare routine to reduce irritation.
How can I treat eczema on the hands?
Eczema on the hands can be caused by frequent handwashing or exposure to irritants. Treatment includes using emollients to keep the skin hydrated, as well as topical corticosteroids to reduce inflammation. Wearing gloves while handling irritating substances can also help prevent flare-ups.
What is the difference between dermatitis and eczema?
Dermatitis and eczema are terms often used interchangeably to describe skin inflammation. However, dermatitis typically refers to any inflammation of the skin, while eczema specifically refers to atopic dermatitis, a chronic condition that is more common in people with a family history of allergies.
Final Thoughts
Eczema is a challenging condition that requires ongoing management and attention. While there is no cure, treatments such as topical steroids, moisturizers, and specific medications can help control flare-ups and improve skin health. Understanding the different types of eczema, their symptoms, and effective treatments can empower individuals to take control of their condition and improve their quality of life. Consulting with a healthcare provider is essential to tailor treatments to individual needs and ensure proper care.